In a medical setting, hard skills such as skill in medical coding, insurance claim processing, and knowledge of referral management systems are essential for accurate patient referrals.
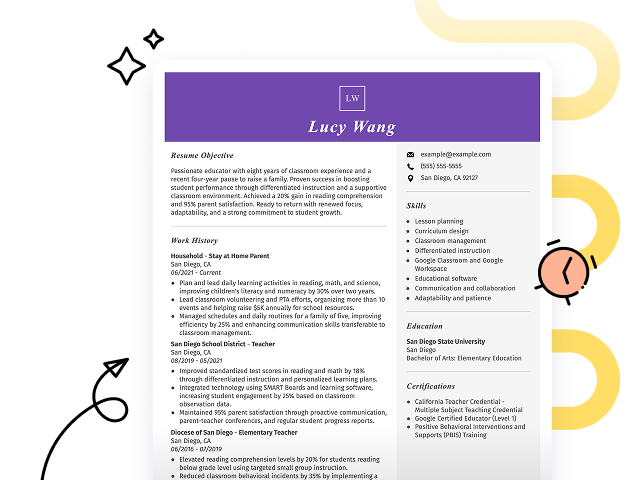
Popular Referral Specialist Resume Examples
Check out our top referral specialist resume examples that emphasize key skills such as patient communication, administrative support, and attention to detail. These examples will help you effectively highlight your accomplishments to potential employers.
Want to build your standout resume? Our Resume Builder offers user-friendly templates specifically designed for professionals in the healthcare field, making your job search easier.
Recommended
Entry-level referral specialist resume
This entry-level resume effectively highlights the job seeker's expertise in managing healthcare referral processes and improving operational efficiency through data analysis and collaboration. New professionals in this field must demonstrate strong organizational skills and a commitment to patient satisfaction, showcasing their ability to improve healthcare delivery despite limited direct experience.
Mid-career referral specialist resume
This resume effectively showcases the job seeker's qualifications by emphasizing their success in client relations and process improvements. The structured presentation of achievements indicates strong readiness for advanced roles, reflecting a solid trajectory in referral management and healthcare coordination.
Experienced referral specialist resume
This resume's work history section effectively demonstrates the applicant's expertise as a referral specialist, showcasing a 35% increase in referral efficiency and a 15% boost in patient satisfaction ratings. The clear bullet point format improves readability, making it easy for hiring managers to quickly identify key achievements.
Resume Template—Easy to Copy & Paste
Yuki Rodriguez
Maplewood, NJ 07048
(555)555-5555
Yuki.Rodriguez@example.com
Professional Summary
A seasoned Referral Specialist with over 9 years of expertise in optimizing patient referral systems. Proven track record of improving referral processes, enhancing patient satisfaction, and spearheading communication initiatives. Skilled in project management, healthcare management, and data analysis for process improvement.
Work History
Referral Specialist
ConnectCare Solutions - Maplewood, NJ
July 2022 - November 2025
- Increased referrals by 20% Q2 2023
- Maintained 98% patient satisfaction
- Processed 300+ referrals monthly
Patient Referral Coordinator
HealthLink Network - Maplewood, NJ
February 2018 - June 2022
- Managed referral backlog, reduced by 35%
- Trained staff to optimize referral process
- Generated monthly reports for management
Referral Liaison
WellCare Associates - Maplewood, NJ
November 2016 - January 2018
- Assisted in 500+ patient referrals yearly
- Improved communication with providers
- Implemented tracking system efficiency
Skills
- Patient Referral Management
- Healthcare Communication
- Data Analysis
- Conflict Resolution
- Process Improvement
- Customer Service
- Healthcare Compliance
- Project Coordination
Certifications
- Certified Healthcare Referral Specialist - National Board for Healthcare Communication
- Project Management in Healthcare - Healthcare Project Management Institute
Education
Master of Health Administration Healthcare Management
University of Wisconsin Madison, Wisconsin
May 2016
Bachelor of Science Business Administration
Northern Illinois University DeKalb, Illinois
May 2014
Languages
- Spanish - Beginner (A1)
- French - Intermediate (B1)
- German - Beginner (A1)
How to Write a Referral Specialist Resume Summary
Your resume summary is the initial touchpoint for hiring managers, making it important to establish a compelling first impression. For a referral specialist, this section should showcase your communication skills and ability to connect patients with appropriate services effectively.
Highlight your expertise in managing referrals, understanding insurance processes, and coordinating with healthcare providers. These key elements demonstrate your value in facilitating patient care and improving operational efficiency.
To clarify what makes an strong summary, consider the following examples that will illustrate both effective strategies and common pitfalls:
I am a dedicated referral specialist with years of experience looking for a new opportunity. I believe my skills in managing patient referrals and coordinating care can be useful to any organization. Ideally, I want to work somewhere that values teamwork and supports career development.
- Lacks specific examples of skills or achievements relevant to the referral specialist role
- Focuses on what the job seeker is seeking rather than emphasizing how they can benefit the employer
- Uses generic phrases like "dedicated" and "years of experience" without demonstrating actual value or impact
Detail-oriented referral specialist with over 4 years of experience in healthcare administration, adept at processing patient referrals and improving care coordination. Achieved a 20% increase in timely referrals by streamlining communication between departments and implementing an electronic tracking system. Proficient in data management, insurance verification, and patient advocacy to improve service delivery.
- Begins with specific experience level and relevant role focus
- Highlights a quantifiable achievement that showcases the ability to improve operational efficiency
- Includes essential technical skills that are important for a referral specialist position
Pro Tip
Showcasing Your Work Experience
The work experience section is important for your resume as a referral specialist, serving as the primary focus of your content. Good resume templates always prioritize this section to effectively showcase your qualifications.
This part should be organized in reverse-chronological order, detailing each past position you've held. Use bullet points to highlight key achievements and responsibilities that demonstrate your expertise in referral management.
To further guide you, we’ll present examples that illustrate effective entries for a referral specialist's work history. These examples will clarify what elevates a resume and what pitfalls to avoid:
Referral Specialist
Health Services Inc. – Atlanta, GA
- Managed patient referrals
- Communicated with healthcare providers
- Handled administrative tasks
- Maintained patient records
- Lacks specific employment dates for context
- Bullet points are overly general and do not highlight any achievements
- Emphasizes routine duties rather than compelling contributions or measurable outcomes
Referral Specialist
Healthcare Solutions Inc. – Atlanta, GA
March 2020 - Present
- Coordinate patient referrals to specialists, improving access to care and improving patient satisfaction scores by 30%
- Streamline referral processes which reduced wait times by 40%, leading to timely treatment for patients
- Develop training materials for new staff on referral procedures, resulting in a 50% decrease in processing errors
- Starts each bullet with powerful action verbs that clearly communicate the job seeker’s achievements
- Incorporates specific metrics demonstrating the effectiveness of initiatives undertaken
- Highlights relevant skills essential for success in the role of referral specialist
While your resume summary and work experience are important components, don't overlook the importance of other sections. Each part plays a role in showcasing your qualifications. For more detailed guidance on crafting an effective resume, be sure to check out our comprehensive guide on how to write a resume.
Top Skills to Include on Your Resume
A well-defined skills section is important for making your resume stand out to potential employers. It quickly showcases your qualifications, allowing hiring managers to see at a glance if you fit their needs.
Employers seek well-rounded professionals who combine strong technical abilities with effective interpersonal skills. Highlight both your hard and soft skills on your resume to show you can contribute expertise while working seamlessly with others.
On the other hand, soft skills like strong communication, attention to detail, and problem-solving abilities play a key role in fostering collaboration with healthcare teams and improving patient experiences.
Choosing the resume skills that align with employer expectations and navigate automated screening systems is important. Many companies use software to filter out applicants who do not possess critical skills required for the role.
To boost your chances, carefully review job postings to gain insights into which skills are prioritized by recruiters and ATS. This approach will enable you to tailor your resume effectively, emphasizing your qualifications and improving visibility in the hiring process.
Pro Tip
10 skills that appear on successful referral specialist resumes
Elevate your resume to attract recruiters by highlighting essential skills for referral specialists. Our resume examples showcase these skills in action, helping you apply with the assurance that a strong resume provides.
Here are 10 key skills you should think about adding to your resume if they align with your background and job expectations:
Attention to detail
Customer service
Data entry skills
Problem-solving abilities
Interpersonal communication
Knowledge of healthcare regulations
Time management
Conflict resolution
Team collaboration
Adaptability
Based on analysis of 5,000+ medical professional resumes from 2023-2024
Resume Format Examples
Choosing the right resume format is important for a referral specialist as it showcases key skills, relevant experience, and career growth in a clear and effective manner.
Functional
Focuses on skills rather than previous jobs
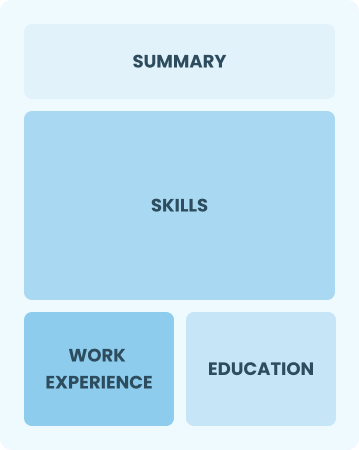
Best for:
Recent graduates and career changers with little to no experience
Combination
Balances skills and work history equally
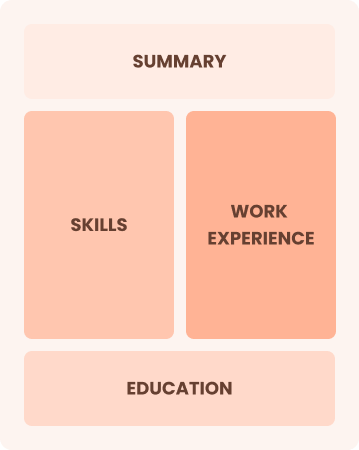
Best for:
Mid-career professionals focused on demonstrating their skills and career progression
Chronological
Emphasizes work history in reverse order

Best for:
Seasoned experts excelling in complex patient referrals and care coordination
Frequently Asked Questions
Should I include a cover letter with my referral specialist resume?
Absolutely, adding a cover letter can significantly improve your application by showcasing your personality and detailing your qualifications. It offers the chance to connect your experience directly to the job at hand. If you need assistance, explore our resources on how to write a cover letter or use our easy-to-navigate Cover Letter Generator for quick results.
Can I use a resume if I’m applying internationally, or do I need a CV?
A CV is typically used instead of a resume for international job applications, especially in Europe and Asia. To create an effective CV, explore our comprehensive resources that outline how to write a CV with proper formatting and essential tips. Additionally, reviewing CV examples can help you craft a standout document.
What soft skills are important for referral specialists?
Soft skills such as communication, problem-solving, and empathy are essential for referral specialists. These interpersonal skills help you coordinate care effectively and build trust with both patients and healthcare providers, leading to a smoother referral process and an improved patient experience.
I’m transitioning from another field. How should I highlight my experience?
Highlight your transferable skills such as communication, organization, and teamwork from previous roles. These abilities illustrate your potential to excel in a referral specialist position, even if you lack direct experience. Share specific instances where these skills led to successful outcomes, linking them to the demands of the new role to show your readiness.
How should I format a cover letter for a referral specialist job?
To format a cover letter for a referral specialist position, begin with your contact details. Follow this with a professional greeting and an engaging introduction that highlights your interest in the role. Clearly outline your relevant qualifications and experience. Tailor each section to match the job requirements, and conclude with a strong call to action encouraging further discussion.
Should I use a cover letter template?
Yes, leveraging a cover letter template for a referral specialist role ensures clear organization. It emphasizes skills like patient navigation and insurance coordination while highlighting achievements in improving referral efficiency and patient satisfaction.