Hard skills are specific technical abilities, including knowledge of HR software, payroll processing, and compliance with labor laws, that are essential for efficiently managing administrative tasks.
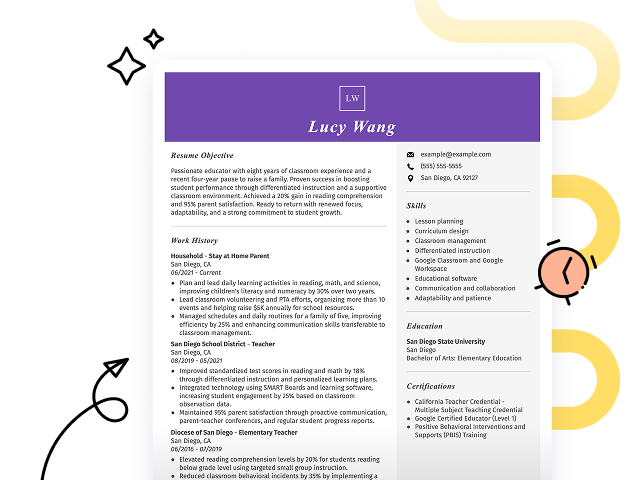
Popular HR Administrator Resume Examples
Discover our top HR administrator resume examples that emphasize key skills such as recruitment, employee relations, and organizational development. These examples illustrate how to effectively showcase your expertise and achievements in the field.
Ready to build your ideal resume? Our Resume Builder offers user-friendly templates specifically designed for human resources professionals, helping you make a lasting impression.
Recommended
Entry-level HR administrator resume
This entry-level resume effectively highlights the applicant's achievements in employee onboarding and talent management, showcasing their ability to implement strategic initiatives that improve organizational efficiency. New professionals in this field must demonstrate practical skills and accomplishments through quantifiable results on their resumes, even if they have limited direct work experience.
Mid-career HR administrator resume
This resume effectively highlights the applicant's qualifications through quantified achievements and diverse HR experiences. The clear progression from assistant to administrator demonstrates an upward trajectory, showcasing readiness for increased responsibilities and leadership in human resources.
Experienced HR administrator resume
This resume's work history section illustrates the applicant's extensive experience in HR, emphasizing significant achievements such as streamlining onboarding by 30% and improving employee engagement by 20%. The bullet-point format improves readability, making it easy for hiring managers to quickly identify key contributions.
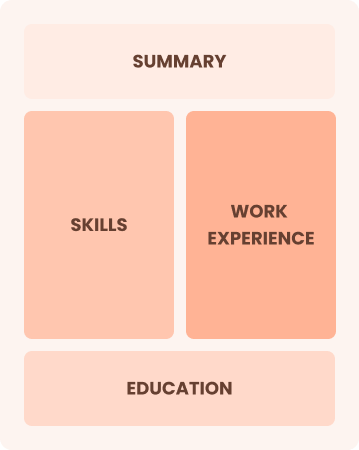
Resume Template—Easy to Copy & Paste
Aya Martinez
Westbrook, ME 04100
(555)555-5555
Aya.Martinez@example.com
Professional Summary
Experienced HR Administrator with a proven track record in reducing turnover by 15% and leading large-scale recruitment strategies. Skilled in employee relations and performance management, ensuring effective HR practices.
Work History
HR Administrator
Professional Talent Solutions - Westbrook, ME
January 2023 - October 2025
- Reduced turnover by 15% through new policies
- Managed 200+ personnel records seamlessly
- Conducted 100+ successful recruitments
HR Coordinator
People Dynamics Inc - Portland, ME
January 2021 - December 2022
- Improved onboarding by 10% efficiency
- Co-led benefits program affecting 300 staff
- Managed 3 major employee satisfaction surveys
Recruitment Specialist
TalentHub Agency - Portland, ME
January 2020 - December 2020
- Sourced candidates, increasing talent pool by 25%
- Executed 50+ hiring strategy plans
- Improved time-to-hire rate by 20%
Skills
- Employee Relations
- Recruitment Strategies
- Performance Management
- HRIS Systems
- Change Management
- Talent Acquisition
- Conflict Resolution
- Benefits Administration
Certifications
- Certified Human Resources Professional - HR Certification Institute
- Strategic HR Leadership - Society for Human Resource Management
Education
Master of Business Administration Human Resources
University of Michigan Ann Arbor, MI
May 2019
Bachelor of Arts Psychology
New York University New York, NY
May 2017
Languages
- Spanish - Beginner (A1)
- French - Intermediate (B1)
- Mandarin - Beginner (A1)
How to Write an HR Administrator Resume Summary
Your resume summary is the first thing employers will see, making it important to create a lasting impression that highlights your fit for the HR administrator role. This section should showcase your skills in managing employee relations, recruitment, and organizational policies.
As an HR administrator, you need to emphasize your skill in communication, problem-solving, and multitasking. These qualifications demonstrate your ability to support a dynamic workforce effectively.
To illustrate what works well in this section, consider the following HR administrator resume summary examples. They will guide you in crafting a compelling summary that attracts attention:
I am an HR administrator with extensive experience in human resources. I seek a position that will allow me to use my skills and advance my career. I am looking for a company that values employee development and offers opportunities for professional growth. I believe I can be a valuable asset to your team if given the chance.
- Contains broad statements about experience without concrete examples or achievements
- Overemphasizes personal goals rather than highlighting contributions to potential employers
- Lacks specific details about skills or expertise relevant to the HR field
Detail-oriented HR Administrator with over 6 years of experience in employee relations and talent acquisition. Successfully improved recruitment efficiency by 30% through the implementation of an applicant tracking system and streamlined onboarding processes. Proficient in HRIS, benefits administration, and compliance with labor laws, ensuring a positive workplace culture.
- Starts with specific years of experience and areas of focus within HR
- Highlights quantifiable achievements that illustrate significant impact on recruitment process efficiency
- Mentions relevant technical skills and competencies that align with HR roles
Pro Tip
Showcasing Your Work Experience
The work experience section is an important part of your resume as an HR administrator. This is where you'll present the bulk of your content, and effective resume templates always feature this important section.
This area should be organized in reverse-chronological order, listing your previous positions. Use bullet points to highlight your key achievements and responsibilities in each role.
To illustrate what makes a strong work history section for HR administrators, we will showcase a couple of examples. These examples will clarify what works well and what you might want to avoid:
HR Administrator
ABC Corporation – New York, NY
- Handled employee files and records
- Assisted in recruitment processes
- Coordinated training sessions
- Responded to employee inquiries
- Lacks specific details about accomplishments or impact
- Bullet points are overly simplistic and do not highlight skills
- Does not mention any measurable outcomes or improvements
HR Administrator
ABC Corporation – New York, NY
March 2020 - Present
- Streamline recruitment processes resulting in a 30% reduction in time-to-hire for key positions
- Develop and implement employee training programs that improved staff retention rates by 15% over one year
- Administer HR policies and procedures ensuring compliance with labor laws, improving workplace satisfaction and productivity
- Starts each bullet point with compelling action verbs to highlight the applicant’s contributions
- Incorporates specific metrics showing measurable impact on the organization’s performance
- Demonstrates relevant skills such as compliance and training development essential for HR roles
While your resume summary and work experience are important, it's essential to focus on other sections that create a full picture of your professional self. For detailed tips on crafting every part effectively, be sure to check out how to write a resume.
Top Skills to Include on Your Resume
A skills section is important for your resume as it quickly highlights your qualifications to potential employers. It serves as a snapshot of what you bring to the table, making it easier for hiring managers to see if you fit the role.
As an HR administrator, on showcasing both hard skills and soft skills to prove you're a well-rounded candidate. A balanced mix of hard skills that demonstrate your industry expertise and soft skills that convey your professionalism is key to making a strong impression.
Soft skills, such as communication, problem-solving, and organization, foster a positive workplace culture and improve collaboration among team members.
When selecting skills for your resume, it’s important to align them with what potential employers expect. Many organizations use applicant tracking systems (ATS) that filter out job seekers lacking essential resume skills.
To ensure you highlight the right competencies, carefully review job postings for insights on which skills are most valued. This approach will help you tailor your resume to attract both recruiters and ATS, increasing your chances of landing an interview.
Pro Tip
10 skills that appear on successful HR administrator resumes
Make your resume shine by incorporating high-demand skills for HR administrator roles. You can see these abilities in action through our resume examples, giving you the confidence to apply effectively.
Here are 10 essential skills you should consider adding to your resume if they align with your experience and job requirements::
Communication
Organizational skills
Conflict resolution
Time management
Attention to detail
Skills in HR software
Employee relations expertise
Data analysis
Recruitment strategies
Training and development
Based on analysis of 5,000+ administrative professional resumes from 2023-2024
Resume Format Examples
Selecting the appropriate resume format is important for an HR administrator, as it showcases key skills and experiences clearly, effectively outlining your professional journey and making a strong impression on employers.
Functional
Focuses on skills rather than previous jobs
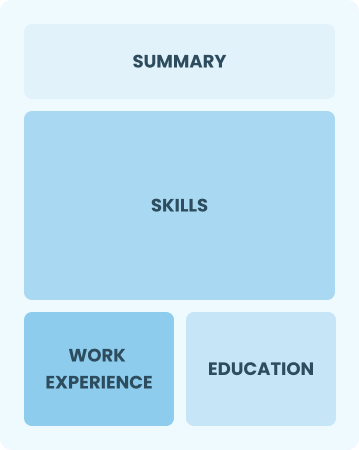
Best for:
Recent graduates and career changers with up to two years of experience
Combination
Balances skills and work history equally
Best for:
Mid-career professionals focused on demonstrating their skills and growth potential
Chronological
Emphasizes work history in reverse order

Best for:
Seasoned HR administrators excelling in strategic workforce management
Frequently Asked Questions
Should I include a cover letter with my HR administrator resume?
Absolutely, including a cover letter can significantly improve your application. It allows you to showcase your personality and highlight specific experiences that relate to the job. For tips on crafting a compelling cover letter, refer to our comprehensive guide on how to write a cover letter. Alternatively, use our Cover Letter Generator for quick assistance. These resources will make the process easier and more effective.
Can I use a resume if I’m applying internationally, or do I need a CV?
When applying for jobs outside the U.S., a CV is typically preferred over a resume. A CV provides a comprehensive overview of your academic and professional history. To assist you, explore our resources on how to write a CV that adheres to international standards. Additionally, review these CV examples for further guidance.
What soft skills are important for HR administrators?
Soft skills like communication, problem-solving, and empathy are essential for HR administrators. These interpersonal skills help build strong relationships with employees and management, enabling effective conflict resolution and promoting a positive workplace culture.
I’m transitioning from another field. How should I highlight my experience?
Highlight your transferable skills such as communication, organization, and conflict resolution when applying for HR administrator roles. These abilities showcase your readiness to adapt and add value even if you have limited direct experience in human resources. Use specific examples from past positions to illustrate how you've successfully handled relevant challenges.
How do I write a resume with no experience?
If you're applying for an HR administrator position but lack formal experience, highlight relevant coursework, internships, or volunteer work. You can showcase these aspects by crafting a resume with no experience. Emphasize skills like organization, communication, and teamwork. Demonstrate your eagerness to learn and adapt, as employers value potential just as much as experience. Your unique perspective can set you apart in this competitive field.
How do I add my resume to LinkedIn?
To improve your resume's visibility on LinkedIn, you should add your resume to LinkedIn by uploading it directly to your profile or detailing key achievements in the "About" and "Experience" sections. This approach helps HR recruiters and hiring managers easily find qualified job seekers who match their needs.