Hard skills are technical, measurable abilities like financial reporting, tax preparation, and skill in accounting software that are essential for accurate financial management.
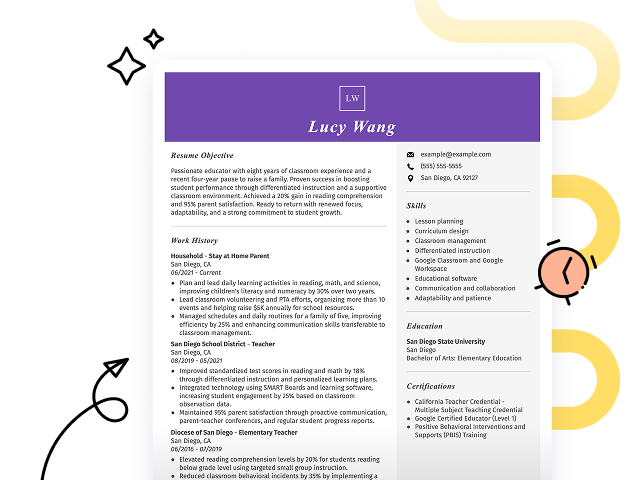
Popular Accounting Resume Examples
Check out our top accounting resume examples that demonstrate key skills such as financial analysis, budgeting, and attention to detail. These examples will help you highlight your accomplishments effectively to potential employers.
Want to make your resume shine? Our Resume Builder offers user-friendly templates specifically designed for accounting professionals, making the process straightforward and efficient.
Recommended
Entry-level accounting resume
This entry-level resume highlights the job seeker's skill in financial reporting and budget management, showcasing significant accomplishments such as reducing account discrepancies and implementing a new budgeting process. New professionals in this field must demonstrate their analytical skills, relevant coursework, and any certifications to reassure employers of their capability despite limited professional experience.
Mid-career accounting resume
This resume effectively showcases a strong background in accounting through clear presentation of qualifications and achievements. The job seeker's progression from junior roles to managerial responsibilities highlights their readiness for leadership positions and complex financial challenges.
Experienced accounting resume
The work experience section illustrates the applicant's exceptional achievements in accounting, highlighting a 15% cost saving and a 20% improvement in budget accuracy. The clear formatting allows quick identification of significant contributions, making it ideal for hiring managers seeking results-oriented applicants.
Resume Template—Easy to Copy & Paste
Li Smith
Brookfield, WI 53008
(555)555-5555
Li.Smith@example.com
Professional Summary
Highly efficient accountant with 7 years of experience. Proven ability to optimize operational budgets, enhance financial strategies, and deliver precise reports. Skilled in audit coordination and strategic planning.
Work History
Accounting
Financial Horizons Inc. - Brookfield, WI
March 2023 - September 2025
- Managed M in annual budgets.
- Increased financial efficiency by 15%.
- Implemented streamlined reporting systems.
Financial Analyst
Precision Investments - Brookfield, WI
January 2020 - February 2023
- Analyzed industry trends to optimize assets.
- Forecasted market changes with 90% accuracy.
- Developed client investment strategies.
Budget Coordinator
Pinnacle Finance Group - Milwaukee, WI
March 2018 - December 2019
- Prepared detailed financial reports quarterly.
- Reduced department costs by 20%.
- Oversaw monthly expense audits.
Skills
- Financial Reporting
- Strategic Planning
- Budget Management
- Data Analysis
- Accounting Software
- Investment Strategies
- Audit Coordination
- Tax Compliance
Education
Master of Business Administration (MBA) Finance
Harvard University Cambridge, Massachusetts
June 2017
Bachelor of Science Accounting
University of California, Berkeley Berkeley, California
June 2015
Certifications
- Certified Financial Analyst - Finance Society of America
- Professional Accounting Certification - Global Accounting Board
Languages
- Spanish - Beginner (A1)
- French - Beginner (A1)
- Mandarin - Beginner (A1)
How to Write an Accounting Resume Summary
Your resume summary is the first thing employers will notice, making it important for creating a strong impression. In this section, you should highlight your key accounting skills and experiences that align with the job requirements.
As an accounting professional, it's essential to showcase your skill in financial analysis, reporting, and compliance. This brief introduction can set the tone for how potential employers perceive your qualifications.
To help you craft an effective resume summary, we’ll explore some examples that illustrate what works well and what doesn’t. These examples will guide you in refining your own summary:
I am an experienced accountant with a solid background and knowledge in the field. I seek a position that allows me to use my skills and contribute positively to your company. A workplace that values professional development and offers a great environment is what I am looking for. I believe I can make a difference if given the chance.
- Contains vague language about experience without providing specific achievements or skills.
- Overuses personal pronouns, making it feel less professional and more casual.
- Emphasizes what the job seeker desires from the job rather than illustrating their value to potential employers.
Detail-oriented accountant with over 7 years of experience in financial reporting and analysis, adept at optimizing processes to improve efficiency. Achieved a 20% reduction in monthly closing time through the implementation of automated reporting tools. Proficient in GAAP, tax compliance, and using ERP systems to streamline operations and ensure accurate financial management.
- Begins with specific experience level and areas of expertise.
- Highlights quantifiable achievement that showcases significant operational improvements.
- Mentions relevant technical skills essential for accounting roles.
Pro Tip
Showcasing Your Work Experience
The work experience section is the centerpiece of your resume in accounting, where you'll find the bulk of your content. The best resume templates always prioritize this section to highlight your professional history.
This area should be structured in reverse-chronological order, providing a clear timeline of your previous roles. Use bullet points to detail your accomplishments and key contributions in each position.
To illustrate effective strategies for presenting your work history, we’ll share a couple of examples that reveal what works well and what pitfalls to avoid:
Accountant
ABC Financial Services – New York, NY
- Handled financial records.
- Prepared reports and statements.
- Collaborated with team members.
- Assisted clients with inquiries.
- Lacks specific information about tasks performed and their impact.
- Bullet points are generic and do not highlight individual achievements.
- Does not mention any tools or software used that could demonstrate expertise.
Accountant
XYZ Financial Services – New York, NY
March 2020 - Current
- Manage financial records for over 100 clients, ensuring accuracy and compliance with GAAP standards.
- Implement cost-saving measures resulting in a 15% reduction in operational expenses within the first year.
- Prepare detailed financial reports that support strategic decision-making for senior management, improving forecasting accuracy by 30%.
- Starts bullet points with dynamic action verbs to clearly convey the applicant's contributions.
- Incorporates quantifiable achievements to highlight the impact made in previous roles.
- Demonstrates relevant technical skills important for accounting professionals through specific examples.
While your resume summary and work experience are important, don't overlook the importance of other sections that can improve your application. To ensure every part of your resume shines, explore our comprehensive guide on how to write a resume.
Top Skills to Include on Your Resume
A skills section is important on your resume as it allows you to showcase your qualifications at a glance. This part of your resume helps employers quickly identify if you possess the essential capabilities they are seeking.
In accounting, it's beneficial to highlight both hard and soft skills. Including both can help you stand out in a competitive job market.
Soft skills include interpersonal qualities such as attention to detail, problem-solving, and effective communication that foster collaboration and ensure clarity in financial operations.
Choosing the right resume skills is important because employers often seek specific qualifications that align with their needs. Additionally, many companies use automated systems to filter out applicants who lack these essential skills.
To effectively tailor your resume, carefully review job postings for insights into the desired competencies. This practice helps ensure you highlight the most relevant skills that will appeal to both recruiters and ATS systems alike.
Pro Tip
10 skills that appear on successful accounting resumes
To attract recruiters' attention, it's important to highlight the high-demand skills relevant to accounting positions. You can see these skills effectively showcased in our resume examples, which will help you present a professional image that stands out.
By the way, consider incorporating these 10 essential skills into your resume if they align with your qualifications and job requirements:
Attention to detail
Analytical thinking
Skill in accounting software
Financial reporting
Tax preparation
Budgeting
Regulatory compliance
Problem-solving
Time management
Interpersonal communication
Based on analysis of 5,000+ accounting professional resumes from 2023-2024
Frequently Asked Questions
Should I include a cover letter with my accounting resume?
Absolutely. Including a cover letter is a fantastic way to highlight your qualifications and show your enthusiasm for the position. A well-crafted cover letter can set you apart from other applicants by adding personal context to your resume. If you need assistance, check our resources on how to write a cover letter or use our Cover Letter Generator for quick, professional results.
Can I use a resume if I’m applying internationally, or do I need a CV?
When applying for jobs outside the U.S., use a CV instead of a resume to showcase your academic and professional history in detail. Explore our comprehensive resources on CV examples and how to write a CV to ensure your application meets international expectations.
What soft skills are important for accountings?
Soft skills are interpersonal skills like communication, problem-solving, and teamwork, all of which are essential in accounting. These skills help professionals convey complex financial information clearly to clients and collaborate effectively within teams, fostering trust and ensuring accurate financial decision-making.
I’m transitioning from another field. How should I highlight my experience?
Highlight your transferable skills such as organization, analytical thinking, and teamwork when applying for accounting roles. These abilities demonstrate your potential to excel in the field despite limited direct experience. Use concrete examples from your past work to illustrate how these strengths can contribute to financial analysis, reporting, and overall team success.
How should I format a cover letter for an accounting job?
To format a cover letter effectively, start with your contact details. Next, include a professional greeting and an engaging opening paragraph that grabs attention. Relate your qualifications to the job description in the summary. Personalize your content for each position you apply for, ensuring you end with a strong call to action.
Should I use a cover letter template?
Yes, using a cover letter template tailored for accounting professionals can improve your letter's structure. This approach ensures you effectively highlight key skills such as financial analysis, attention to detail, and skill in accounting software, making it easier for hiring managers to recognize your qualifications.