Expertise in hard skills like coding, billing software, and understanding healthcare regulations ensures accurate and compliant billing processes.
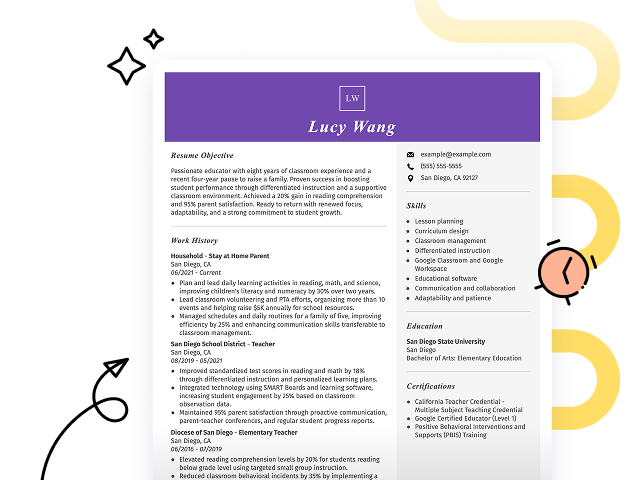
Popular Billing Manager Resume Examples
Check out our top billing manager resume examples that emphasize critical skills such as financial analysis, team leadership, and compliance management. These examples can help you effectively showcase your professional achievements.
Ready to build your ideal resume? Our Resume Builder offers user-friendly templates specifically designed to highlight the expertise of billing professionals.
Recommended
Billing manager resume
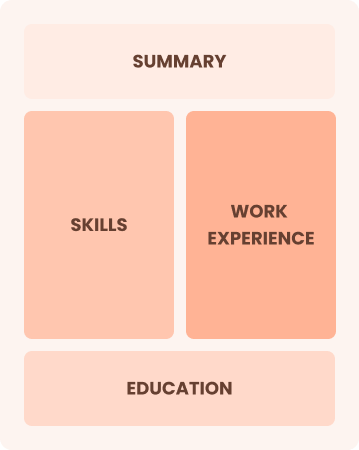
The resume uses a structured layout and resume fonts that improve readability. These design choices not only present the job seeker's qualifications effectively but also reflect careful attention to detail, leaving a positive impression on potential employers.
Revenue manager resume
This resume successfully integrates key skills like revenue management and financial analysis with substantial work experience. By demonstrating these competencies alongside detailed job responsibilities, employers can clearly evaluate the job seeker's effectiveness in improving profitability and making strategic decisions in previous roles.
Medical billing manager resume
This resume skillfully uses bullet points to distill extensive experience into clear, digestible segments, allowing hiring managers to quickly assess qualifications. Thoughtful spacing and organized sections improve readability, ensuring standout accomplishments and metrics are easily identifiable at a glance.
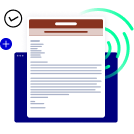
Resume Template—Easy to Copy & Paste
Ming Chen
Portland, OR 97210
(555)555-5555
Ming.Chen@example.com
Professional Summary
Experienced Billing Manager with expertise in financial reporting, accounts receivable, and billing software. Proven track record of improving billing accuracy and reducing overdue accounts while leading high-performing teams.
Work History
Billing Manager
Metro Health Systems - Portland, OR
January 2023 - November 2025
- Improved billing accuracy by 25%
- Reduced overdue accounts by 15%
- Trained team on billing software
Accounts Receivable Coordinator
Pine Valley Medical - Portland, OR
January 2020 - December 2022
- Managed accounts worth M
- Collected 30% overdue payments
- Streamlined billing process
Billing Specialist
Riverdale Clinics - Portland, OR
January 2018 - December 2019
- Processed 150 invoices monthly
- Resolved billing issues within 24hrs
- Maintained 98% billing accuracy
Skills
- Billing Management
- Accounts Receivable
- Financial Reporting
- Team Leadership
- Billing Software
- Budgeting
- Data Analysis
- Customer Service
Certifications
- Certified Billing Professional - National Association of Billing Professionals
- Certified Medical Billing Specialist - AAPC
Education
Master of Business Administration Accounting
University of New York New York, NY
May 2016
Bachelor of Science Finance
State University of New York Albany, NY
May 2014
Languages
- Spanish - Beginner (A1)
- French - Beginner (A1)
- German - Beginner (A1)
How to Write a Billing Manager Resume Summary
Your resume summary is the first impression hiring managers will have of you, making it important to present your qualifications effectively. As a billing manager, it's essential to highlight your expertise in financial processes and team leadership within the healthcare or business sectors. The following examples will illustrate what makes a strong resume summary for this role and help you identify effective strategies:
I am an experienced billing manager with many years in the field. I am seeking a position where I can apply my skills and help the company succeed. A job that offers good benefits and chances to advance is what I’m looking for. I believe I can contribute positively if given the chance.
- Lacks specific examples of skills or achievements relevant to billing management
- Overuses personal language, making it feel less professional and more casual
- Emphasizes what the job seeker seeks rather than detailing how their experience can benefit the employer
Results-driven billing manager with over 7 years of experience in healthcare billing and revenue cycle management. Achieved a 20% reduction in claim denials through process optimization and staff training initiatives. Proficient in using electronic billing systems, CPT coding, and compliance regulations to ensure accurate and timely billing processes.
- Begins by clearly stating the applicant's experience level and industry focus
- Highlights a specific quantifiable achievement that illustrates their impact on the organization's financial performance
- Demonstrates relevant technical skills and competencies important for effective billing management
Pro Tip
Showcasing Your Work Experience
The work experience section is important for your resume as a billing manager, serving as the main focus where you’ll provide most of your content. Good resume templates always prioritize this important section.
This part should be organized in reverse-chronological order, detailing your previous positions. Use bullet points to highlight key achievements and responsibilities that demonstrate your expertise in billing management.
To further illustrate effective approaches, we’ll present a couple of examples that showcase what works well and what should be avoided in this section:
Billing Manager
Summit Healthcare Solutions – Los Angeles, CA
- Managed billing processes
- Handled customer inquiries and complaints
- Worked with insurance companies
- Maintained records and reports
- Lacks employment dates for context
- Bullet points are too generic and do not highlight accomplishments
- Focuses on routine tasks instead of measurable results that demonstrate impact
Billing Manager
Summit Healthcare Solutions – San Francisco, CA
March 2020 - Present
- Oversee billing operations for a team of 10, ensuring timely submission of claims and reducing denial rates by 30%
- Implement streamlined processes that improved monthly revenue cycle reporting accuracy by 25%, improving financial visibility
- Train and mentor staff on compliance regulations and best practices, resulting in a 40% increase in departmental efficiency
- Starts each bullet with strong action verbs that directly highlight the job seeker's achievements
- Incorporates specific metrics to quantify success and showcase effectiveness
- Demonstrates relevant expertise in billing management through detailed descriptions of responsibilities and outcomes
While your resume summary and work experience are important, don’t overlook other key sections that can improve your candidacy. Ensuring every part of your resume is polished is essential for making a strong impression. For detailed guidance on crafting the perfect resume, refer to our comprehensive guide on how to write a resume.
Top Skills to Include on Your Resume
A skills section on your resume is important for showcasing job-relevant skills at a glance. It helps employers quickly identify if you possess the essential abilities they need.
Employers look for professionals who bring together strong technical abilities and the interpersonal skills needed to collaborate and communicate effectively. Show both your hard and soft skills on your resume to present a balanced, well-rounded profile.
Meanwhile, soft skills such as strong communication, attention to detail, and problem-solving abilities foster effective collaboration with healthcare teams and improve the patient experience through clear financial guidance.
Selecting the right resume skills is important because employers seek applicants who align with their expectations. Additionally, many companies use automated screening systems that filter out applicants lacking essential skills for the role.
To effectively capture a recruiter's attention, carefully review job postings to identify which skills are emphasized. This strategy will not only help you tailor your resume but also ensure it meets the criteria set by ATS systems.
Pro Tip
10 skills that appear on successful billing manager resumes
Boost your resume's visibility to hiring managers by highlighting essential skills that billing managers frequently use. These high-demand abilities can be found in our resume examples, providing you with a template for success.
Here are 10 skills you should consider including in your resume if they align with your qualifications and job expectations:
Attention to detail
Analytical thinking
Problem-solving
Communication skills
Time management
Expertise in billing software
Knowledge of healthcare regulations
Customer service orientation
Team collaboration
Financial reporting
Based on analysis of 5,000+ management professional resumes from 2023-2024
Resume Format Examples
Selecting the right resume format for a billing manager is important because it highlights your financial expertise, relevant experience, and career growth in a clear and strong way.
Functional
Focuses on skills rather than previous jobs
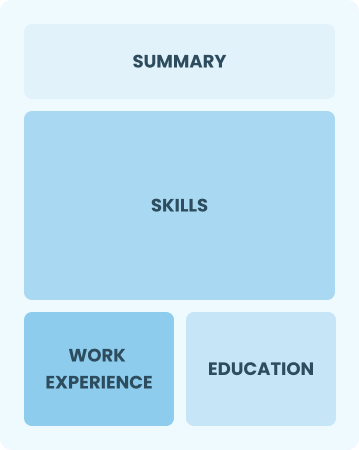
Best for:
Recent graduates and career changers with up to two years of experience
Combination
Balances skills and work history equally
Best for:
Mid-career professionals focused on demonstrating their skills and potential for growth
Chronological
Emphasizes work history in reverse order

Best for:
Seasoned leaders in billing operations and strategic revenue management
Frequently Asked Questions
Should I include a cover letter with my billing manager resume?
Absolutely, including a cover letter can significantly improve your application. It offers you the chance to highlight your unique qualifications and convey your enthusiasm for the position. For those unsure of how to craft one, we recommend checking out our guide on how to write a cover letter or using our Cover Letter Generator to simplify the process.
Can I use a resume if I’m applying internationally, or do I need a CV?
When applying for jobs internationally, it's often best to use a CV instead of a resume. A CV provides detailed information about your academic and professional history, making it suitable for many countries' hiring practices. To ensure your application stands out, explore our resources on how to write a CV and review various CV examples for formatting and creation guidance.
What soft skills are important for billing managers?
Soft skills like attention to detail, problem-solving, and interpersonal skills are essential for billing managers. These abilities assist in resolving discrepancies, ensuring accurate invoicing, and maintaining positive relationships with clients and team members.
I’m transitioning from another field. How should I highlight my experience?
When applying for billing manager roles, highlight your transferable skills such as communication, organization, and analytical thinking. These abilities can demonstrate your potential to excel in this position even if your experience is in a different field. Provide specific examples from your past work that relate directly to managing billing processes or improving efficiency.
How should I format a cover letter for a billing manager job?
To format a cover letter for billing manager positions, begin with your contact information and include a warm greeting. Follow this with an engaging introduction that highlights your interest in the role and summarizes your key qualifications. Each section should be tailored to the specific job description, ensuring relevance and clarity. Conclude with a strong call to action.
How do I write a resume with no experience?
Even if you have limited work experience as a billing manager, you can showcase relevant skills like attention to detail, organization, and skill with billing software. Highlight any internships, coursework, or projects that involved financial management or customer service. For tips on crafting a resume with no experience, your enthusiasm for the role and willingness to learn will resonate with employers.