City, State, Zip Code
Home: 000-000-0000 | Cell: 000-000-0000
email@email.com
Skilled and experienced Revenue Cycle Specialist has strong knowledge of medical billing practices.Knowledgeable about insurance company and government program reimbursements.Has a technical Certificate in Medical Billing and Coding as well as AAHAM certification as a Certified Revenue Cycle Specialist.
- Good ability to interpret rules and regulations set by Medicaid Medicare and commercial insurance payors
- Strong medical bill collections practice
- Highly organized with strong attention to detail
- Ability to self-motivate and work with minimal supervision
- Excellent oral and written communication skills
- Thorough knowledge concerning patient confidentiality and HIPAA rules
- Analyzed account receivables and corrected all problems.
- Met all productivity and collection goals including dollars collected and accounts handled.
- Initiated appeals of denial of payment for services.
- Reduced rates of delinquent accounts.
- Set up payment plans for people with delinquent medical bills.
- Made calls to insurance companies and individuals with outstanding accounts and arranged payments.
- Documented all activities.
- Maintained patient confidentiality and followed the mandates of HIPAA and the FDCPA.
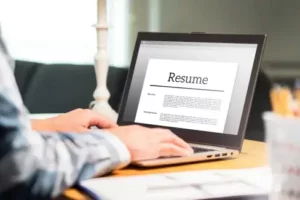
There are plenty of opportunities to land a Revenue Cycle Specialist job position, but it won’t just be handed to you. Crafting a Revenue Cycle Specialist resume that catches the attention of hiring managers is paramount to getting the job, and LiveCareer is here to help you stand out from the competition.
Featured in:*

*The names and logos of the companies referred to in this page are all trademarks of their respective holders. Unless specifically stated otherwise, such references are not intended to imply any affiliation or association with LiveCareer.