Hard skills include expertise in medical billing, coding accuracy, and knowledge of insurance policies that ensure timely reimbursement for healthcare services.
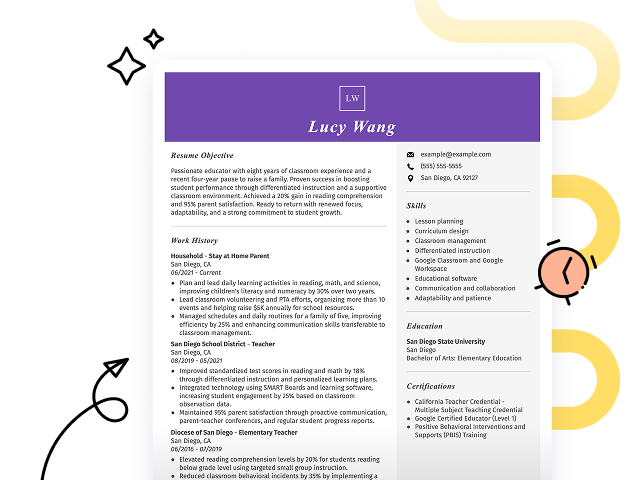
Popular Field Reimbursement Manager Resume Examples
Discover our top field reimbursement manager resume examples that emphasize critical skills such as claims management, regulatory compliance, and effective communication. These examples can help you showcase your qualifications in a way that appeals to employers.
Ready to develop a winning resume? Our Resume Builder offers user-friendly templates designed specifically for professionals in the reimbursement field, helping you make a strong impression.
Recommended
Entry-level field reimbursement manager resume
This entry-level resume effectively highlights the applicant's achievements in improving reimbursement efficiency and managing claims, showcasing their strong analytical skills and leadership capabilities. New professionals in this field must clearly illustrate their problem-solving abilities and relevant accomplishments, even with limited experience, to attract potential employers.
Mid-career field reimbursement manager resume
This resume effectively showcases qualifications through quantifiable achievements and progressive responsibilities, positioning the applicant as a capable leader ready to tackle complex challenges in healthcare reimbursement management.
Experienced field reimbursement manager resume
This resume's work history section illustrates the applicant's significant impact as a field reimbursement manager, with achievements such as improving approval rates by 20% and generating an additional $500K in revenue yearly. The clear formatting allows hiring managers to quickly grasp key accomplishments and qualifications.
Resume Template—Easy to Copy & Paste
Yuki Liu
Lakeside, CA 92050
(555)555-5555
Yuki.Liu@example.com
Skills
- Healthcare reimbursement
- Revenue cycle management
- Claim processing
- Analytical skills
- Problem-solving
- Team leadership
- Process optimization
- Communication skills
Certifications
- Certified Professional Coder - American Academy of Professional Coders
- Healthcare Reimbursement Specialist - Healthcare Financial Management Association
Languages
- Spanish - Intermediate (B1)
- French - Beginner (A1)
- German - Beginner (A1)
Professional Summary
Results-driven Field Reimbursement Manager with expertise in healthcare reimbursement processes, strong analytical skills, and proven track record in revenue cycle management, seeks to optimize claim accuracy and improve revenue flow efficiency.
Work History
Field Reimbursement Manager
Medical Access Solutions - Lakeside, CA
November 2023 - November 2025
- Increased reimbursement rate by 15%
- Reduced denials by 100K annually
- Streamlined 10 provider coordination
Reimbursement Analyst
HealthWorks Insights - San Francisco, CA
November 2020 - November 2023
- Implemented system changes saving 150K
- Improved claim accuracy by 20%
- Trained 8 team members
Billing Coordinator
OptimalCare Management - San Diego, CA
November 2018 - November 2020
- Processed claims, increasing revenue by 12%
- Minimized errors by 30%
- Supported 5 departments
Education
Master of Health Administration Health Services
University of Illinois Chicago, Illinois
May 2018
Bachelor of Science Business Administration
Ohio State University Columbus, Ohio
May 2016
How to Write a Field Reimbursement Manager Resume Summary
Your resume summary is the first opportunity to captivate hiring managers, setting the tone for your application. As a field reimbursement manager, you should highlight your expertise in navigating complex reimbursement processes and your ability to drive results.
In this role, showcasing your analytical skills and attention to detail is essential. You need to demonstrate how you effectively manage claims and collaborate with various stakeholders to ensure compliance and optimize revenue.
To illustrate what works well, we’ll look at some resume summary examples that can guide you in crafting a standout introduction:
I am a skilled field reimbursement manager with extensive experience in the healthcare sector. I seek a position that allows me to use my expertise and contribute to the company's success. A role with good benefits and career advancement is what I’m looking for, as I believe I can add value to any team.
- Lacks specific examples of achievements or skills relevant to field reimbursement management
- Overuses personal pronouns and does not provide concrete information about contributions
- Emphasizes what the job seeker desires from the job rather than showcasing how they can benefit the employer
Results-driven Field Reimbursement Manager with over 7 years of experience in healthcare reimbursement processes, specializing in claims management and payer relations. Successfully improved claim approval rates by 20% through streamlined processes and staff training initiatives. Proficient in analyzing payer policies, managing appeals, and using revenue cycle management software to improve operational efficiency.
- Highlights extensive experience specific to the reimbursement field
- Includes quantifiable achievements that showcase measurable impact on claim processing efficiency
- Demonstrates relevant technical skills and competencies that are critical for success in reimbursement management
Pro Tip
Showcasing Your Work Experience
The work experience section is important for your resume as a field reimbursement manager, serving as the main focus of your content. Good resume templates emphasize this area to draw attention to your professional journey.
This section should be organized in reverse-chronological order, detailing your previous roles. Use bullet points to highlight key achievements and contributions relevant to reimbursement management in each position.
To illustrate effective entries, we’ve prepared a couple of examples that showcase what works and what doesn’t in this critical section:
Field Reimbursement Manager
Health Solutions Inc. – Atlanta, GA
- Managed reimbursement claims
- Communicated with clients and insurers
- Reviewed documentation for accuracy
- Handled inquiries related to payments
- Lacks specific accomplishments or metrics to demonstrate impact
- Bullet points are generic and do not highlight unique skills or strengths
- Does not provide any context about the scope of responsibilities or challenges faced
Field Reimbursement Manager
HealthCorp Solutions – Atlanta, GA
March 2020 - Current
- Streamlined reimbursement processes for a portfolio of 15 products, reducing claim denial rates by 30% within one year
- Educated healthcare providers on reimbursement policies through workshops, resulting in a 50% increase in successful claims submissions
- Collaborated with cross-functional teams to develop strategic initiatives that improved overall revenue cycle efficiency by 20%
- Uses action verbs to clearly convey the impact of the applicant's efforts
- Incorporates specific metrics that highlight achievements and improvements
- Demonstrates relevant skills such as education and collaboration critical for the role
While your resume summary and work experience are important components, don’t overlook the importance of other sections. Each part plays an essential role in showcasing your skills and qualifications. For more detailed guidance, be sure to explore our extensive guide on how to write a resume.
Top Skills to Include on Your Resume
A strong skills section is important for your resume, as it allows you to present your qualifications at a glance. This is particularly essential in fields where specific competencies are required, helping you stand out to potential employers.
Employers increasingly expect candidates to bring together strong technical expertise and the interpersonal abilities that keep teams moving. As you craft your resume, highlight both hard and soft skills to show you’re versatile and ready to contribute on multiple levels.
Soft skills encompass problem-solving, communication, and negotiation abilities that foster collaboration with healthcare providers and promote efficient processing of claims, ultimately improving patient care.
Selecting the right resume skills is important for meeting employer expectations and satisfying automated screening systems. Many organizations use software to filter out applicants lacking essential qualifications for the job, making it imperative to align your skills with what employers seek.
To effectively showcase your abilities, review job postings closely. They provide valuable insights into the key skills that recruiters prioritize, ensuring your resume resonates with both hiring managers and ATS algorithms.
Pro Tip
10 skills that appear on successful field reimbursement manager resumes
Highlighting key skills on your resume can significantly improve your appeal to recruiters for field reimbursement manager positions. Our resume examples showcase these essential skills, giving you a solid foundation to create a standout application.
By the way, consider incorporating relevant skills that align with your experience and the job specifications:
Analytical thinking
Attention to detail
Effective negotiation
Project management
Data analysis
Strong communication
Knowledge of insurance regulations
Problem-solving abilities
Team collaboration
Adaptability
Based on analysis of 5,000+ management professional resumes from 2023-2024
Resume Format Examples
Choosing the appropriate resume format is important for a field reimbursement manager as it effectively showcases key skills, relevant experience, and career growth to potential employers.
Functional
Focuses on skills rather than previous jobs
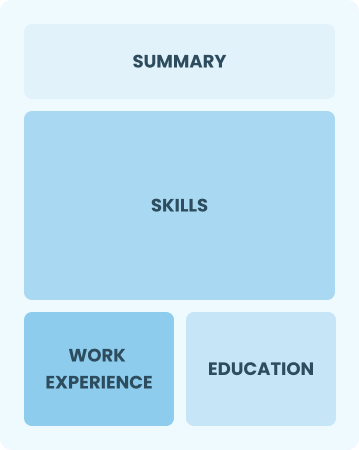
Best for:
Recent graduates and career changers with up to two years of experience
Combination
Balances skills and work history equally
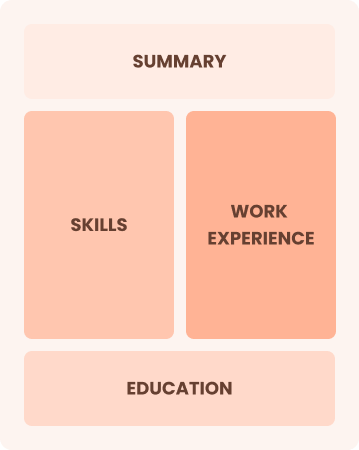
Best for:
Mid-career professionals focused on demonstrating their skills and growth potential
Chronological
Emphasizes work history in reverse order

Best for:
Experienced leaders in healthcare reimbursement strategies and compliance
Frequently Asked Questions
Should I include a cover letter with my field reimbursement manager resume?
Absolutely, including a cover letter is essential for making your application memorable. It gives you a chance to showcase your personality and explain how your skills align with the job. If you're looking for help writing one, explore how to write a cover letter or use our Cover Letter Generator to create a professional letter in no time.
Can I use a resume if I’m applying internationally, or do I need a CV?
As a field reimbursement manager, you may need to create a CV instead of a resume for international applications. Many countries prefer CVs for their detailed format. To help you craft an effective CV, explore our comprehensive resources on how to write a CV and browse through various CV examples tailored to global expectations.
What soft skills are important for field reimbursement managers?
Soft skills like interpersonal skills, including communication, problem-solving, and negotiation, are essential for field reimbursement managers. These abilities enable effective collaboration with healthcare providers and insurers, ensuring smooth processes and strong professional relationships that ultimately improve financial outcomes.
I’m transitioning from another field. How should I highlight my experience?
When applying for field reimbursement manager roles, highlight your transferable skills such as organization, communication, and analytical thinking. These abilities are important in navigating complex reimbursement processes, even if you lack direct experience. Share specific examples from your previous jobs that illustrate how these skills have led to successful outcomes in similar situations.
Should I use a cover letter template?
Using a cover letter template tailored for field reimbursement managers can improve the structure of your application. This approach ensures clarity when presenting key competencies like regulatory compliance and claims management while effectively showcasing relevant achievements such as improved reimbursement processes.
Should I include a personal mission statement on my field reimbursement manager resume?
Including a personal mission statement on your resume is beneficial as it effectively highlights your values and career aspirations. This approach resonates particularly well with organizations that prioritize cultural fit and maintain strong missions aligned with their workforce values.