Hard skills, like skill in using virtual communication tools, data entry accuracy, and customer service software, are essential for efficiently managing client interactions.
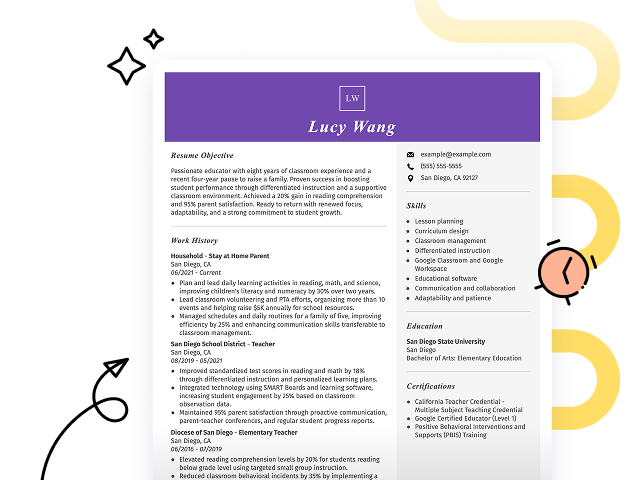
Popular Work At Home Agent Resume Examples
Check out our top work at home agent resume examples that demonstrate key skills like customer service, problem-solving, and time management. These examples will help you showcase your qualifications effectively to potential employers.
Looking to build your own resume? Our Resume Builder offers user-friendly templates specifically designed for remote work professionals, making the process simple and efficient.
Recommended
Entry-level work at home agent resume
This entry-level resume effectively highlights the applicant's achievements in customer service and remote communication, showcasing their ability to improve client satisfaction and streamline processes. New professionals in this field must demonstrate their problem-solving skills and adaptability through specific accomplishments, even when lacking extensive work experience.
Mid-career work at home agent resume
This resume effectively showcases key qualifications by highlighting accomplishments in customer satisfaction and account management. The clear presentation of skills and experiences demonstrates the applicant's readiness for advanced remote roles, reflecting a strong career trajectory in client service excellence.
Experienced work at home agent resume
The work history section highlights the applicant's strong experience as a work at home agent, demonstrating their ability to resolve over 50 customer queries daily and improve satisfaction rates by 18%. The bullet-point format improves readability, making it ideal for hiring managers seeking clear evidence of accomplishments.
Resume Template—Easy to Copy & Paste
Jerry White
Houston, TX 77002
(555)555-5555
Jerry.White@example.com
Professional Summary
Proven Work At Home Agent with expertise in boosting sales and client satisfaction. 9 years in remote support roles across various industries. Adept in data analysis and project management to optimize customer service excellence.
Work History
Work At Home Agent
Connect Solutions Inc. - Houston, TX
January 2023 - December 2025
- Enhanced sales by 30% via strategic upsell
- Resolved 90% of customer issues first contact
- Led 5 major projects improving client retention
Remote Customer Support Specialist
Virtual Assist Co. - The Woodlands, TX
June 2018 - December 2022
- Managed 150 client accounts consistently
- Reduced response time by 25% annually
- Achieved customer satisfaction rate of 95%
Online Service Coordinator
E-Support Systems - Pasadena, TX
June 2016 - May 2018
- Trained 20 remote staff in new software
- Integrated new tools saving 10K yearly
- Improved team efficiency by 40%
Languages
- Spanish - Beginner (A1)
- German - Beginner (A1)
- French - Beginner (A1)
Skills
- Remote work strategies
- Customer service excellence
- Project management
- Data analysis
- Sales optimization
- Team leadership
- Problem-solving
- Communication skills
Certifications
- Certified Customer Support Professional - Customer Service Institute
- Remote Work Management - E-Work Training Solutions
Education
Master's Business Administration
University of Washington Seattle, Washington
June 2015
Bachelor's Marketing
Western Washington University Bellingham, Washington
June 2013
How to Write a Work At Home Agent Resume Summary
Your resume summary is the gateway to making a lasting impression on hiring managers. This section should clearly present your skills and experiences that align with the work-at-home agent role.
In this profession, it's essential to highlight your communication abilities, problem-solving skills, and any relevant customer service experience. These elements will showcase your aptitude for remote work and client interactions.
To illustrate what an effective resume summary looks like, here are some examples that will guide you in crafting your own:
I am an experienced work-at-home agent looking for a position where I can use my skills and contribute to the team. I prefer a job that offers flexibility and a good work environment. I believe I can really help if given the chance.
- Lacks specific achievements or qualifications relevant to the role of a work-at-home agent
- Emphasizes personal preferences instead of showcasing how the job seeker can benefit the employer
- Uses generic phrases that do not highlight unique strengths or experiences, making it less powerful
Results-driven work-at-home agent with over 4 years of experience in customer service, specializing in remote support and issue resolution. Increased customer satisfaction scores by 20% through effective communication strategies and proactive problem-solving techniques. Proficient in CRM software, data entry, and virtual collaboration tools to improve team productivity.
- Begins with concrete experience level and specific area of expertise
- Highlights quantifiable achievement that illustrates a positive impact on customer satisfaction
- Mentions relevant technical skills that are critical for remote work success
Pro Tip
Showcasing Your Work Experience
The work experience section is the centerpiece of your resume as a work at home agent. This is where you’ll provide the bulk of your content, and good resume templates always feature this section prominently.
This area should be organized in reverse-chronological order, listing your previous positions. Use bullet points to highlight specific achievements and skills demonstrated in each role.
To further guide you, we will share a couple of examples that illustrate effective work history entries for work at home agents. These examples will clarify what works well and what may not resonate.
Work at Home Agent
Customer Solutions Inc. – Remote
- Handled customer inquiries
- Resolved issues over the phone
- Documented interactions in the system
- Collaborated with team members online
- Lacks specific employment dates to provide context
- Bullet points describe basic tasks without highlighting achievements
- Does not include measurable outcomes or personal contributions
Work at Home Agent
TeleTech Solutions – Remote
March 2020 - Current
- Manage customer inquiries and provide solutions for product issues, achieving a 95% customer satisfaction rating
- Train new agents on best practices and effective communication skills, contributing to a 15% increase in team efficiency
- Use CRM software to track interactions and follow up with customers, resulting in a 30% reduction in response times
- Starts each bullet point with powerful action verbs that clearly outline contributions
- Incorporates specific metrics that highlight performance outcomes
- Highlights relevant skills essential for the role, showing versatility and effectiveness
While your resume summary and work experience are important components, don't overlook the importance of other sections. Each part of your resume deserves careful consideration to create a well-rounded presentation. For detailed guidance, be sure to check out our comprehensive guide on how to write a resume.
Top Skills to Include on Your Resume
Including a skills section on your resume is important as it highlights your qualifications at a glance. This section allows potential employers to immediately see if you possess the essential abilities required for the role.
As a work-at-home agent, focus on both technical skills and interpersonal abilities. Include familiarity with customer relationship management software, chat platforms, and data entry tools, along with strong communication skills, to demonstrate your effectiveness in a remote work environment.
In addition, soft skills such as strong communication, adaptability, and problem-solving abilities are important for providing effective support and fostering positive relationships with customers remotely. To further explore these competencies, you can delve into a comprehensive list of hard skills.
Selecting the right resume skills is important for aligning with what employers expect from job seekers. Many organizations rely on automated systems to filter applicants, so it’s important to include relevant skills that meet their criteria.
To improve your chances of getting noticed, carefully examine job postings to identify key skills that are emphasized. By tailoring your resume to highlight these specific skills, you can capture the attention of both recruiters and ATS systems alike.
Pro Tip
10 skills that appear on successful work at home agent resumes
Improve your resume to capture the attention of recruiters by incorporating high-demand skills relevant to work at home agent positions. Our resume examples highlight these skills, enabling you to apply for jobs with the professionalism a strong resume provides.
Here are 10 skills you should consider including in your resume if they align with your qualifications and job expectations:
Customer service orientation
Strong communication
Time management
Problem-solving
Technical skill
Adaptability
Attention to detail
Team collaboration
Self-motivation
Conflict resolution
Based on analysis of 5,000+ real estate professional resumes from 2023-2024
Resume Format Examples
Choosing the ideal resume format is important for effectively showcasing your customer service abilities, remote work experience, and professional growth as a work-at-home agent.
Functional
Focuses on skills rather than previous jobs
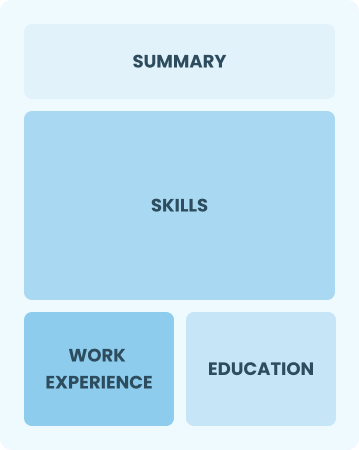
Best for:
Recent graduates and career changers with limited experience seeking flexible work
Combination
Balances skills and work history equally
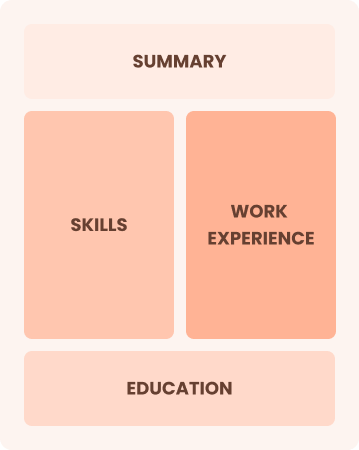
Best for:
Mid-career professionals eager to highlight their skills and growth potential
Chronological
Emphasizes work history in reverse order

Best for:
Seasoned agents excelling in team leadership and client relations
Frequently Asked Questions
Should I include a cover letter with my work at home agent resume?
Absolutely, including a cover letter can improve your application by showcasing your personality and relevant skills. It allows you to elaborate on your experience and demonstrate genuine interest in the position. For assistance, check our guide on how to write a cover letter or use our Cover Letter Generator for quick help tailored to your needs.
Can I use a resume if I’m applying internationally, or do I need a CV?
When applying for jobs abroad, use a CV instead of a resume, as it is often preferred in many countries. To assist you, we offer various resources that provide guidance on how to write a CV and ensure your application meets international standards. Additionally, explore our collection of CV examples to see different formatting and creation styles.
What soft skills are important for work at home agents?
Soft skills like communication, problem-solving, and patience are essential for work-at-home agents. These interpersonal skills help agents interact effectively with customers while fostering a collaborative team environment, which boosts service quality and customer satisfaction.
I’m transitioning from another field. How should I highlight my experience?
Highlight your transferable skills, such as communication, organization, and customer service, when applying for work-at-home agent positions. These abilities demonstrate your readiness to excel in remote settings, even if you lack direct experience. Use concrete examples from past jobs to illustrate how you've successfully addressed client needs or managed tasks effectively.
How should I format a cover letter for a work at home agent job?
To format a cover letter for work at home agent positions, begin with your contact details. Follow this by including a professional greeting and an engaging introduction that highlights your relevant skills. Include specific experiences related to remote work and conclude with a strong closing statement. Tailoring each letter to the job description is essential for making a positive impression.
Should I include a personal mission statement on my work at home agent resume?
Yes, adding a personal mission statement to your resume can effectively showcase your dedication and career aspirations. This approach is especially beneficial when you're applying to companies with a strong customer service focus or a remote work culture.